Documentation through the Perioperative Phases of Care: Postoperative Handover
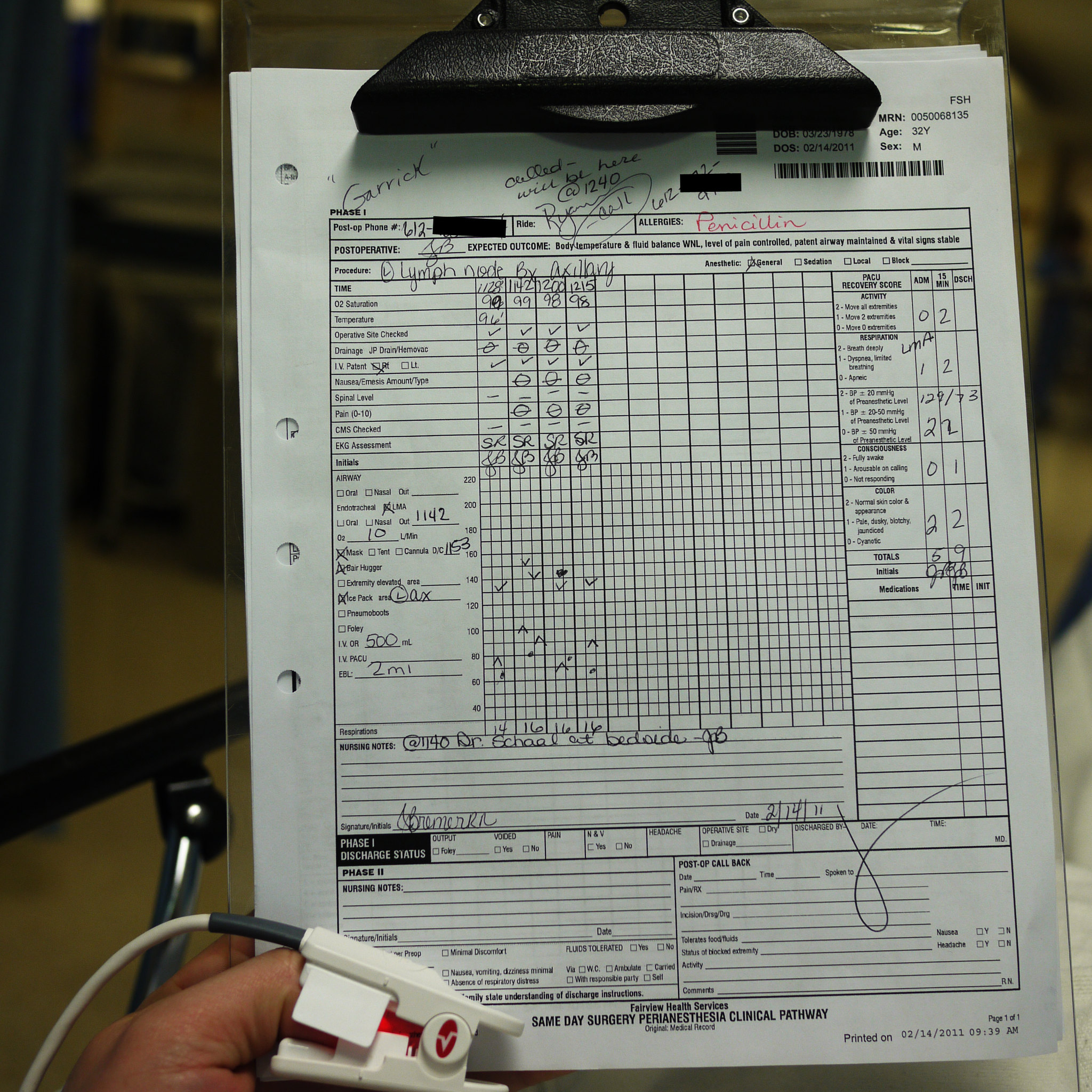
After the surgery is complete, the perioperative nurse helps to transfer the patient to the post-operative recovery unit (PACU). The nurse is responsible for providing a handover report which will be discussed further in course two. The circulating nurse must ensure that during handover, the following documentation is highlighted:
- Patient status (airway, breathing, circulation, hemodynamics, temperature).
- Patient identifiers, weight, age.
- Any allergies.
- Type of anesthesia provided.
- Pertinent diagnosis and medical history, as well as the surgery performed.
- Any intraoperative events or complications that may have occurred.
- Skin condition, including any areas of concern or breakdown during the intraoperative period.
- Intraoperative medications given.
- IV fluids and lines present.
- Drains and catheters present.
- Surgical site information, including any packing, dressing type, and drains.
- Post operative plan.
(AORN, 2021; ORNAC, 2021 – 3.10)

Electronic Documentation
Most facilities use electronic documentation to support the fast-paced workflow. Depending on the facility, these records may be integrated into the electronic charting system or may be printed and added to the patient’s physical chart once the procedure is completed. Perioperative nurses receive training at their home facility in using the electronic charting record.
It is important that all perioperative nurses are trained in ‘downtime’ procedures. There is always a chance that the computer system may require repair or updating. Having a paper backup charting system is essential to ensure that all data and information related to the surgery is captured. Each hospital facility must have a procedure for downtime paper charting and recovery of data once the computer system is functional.
Hospitals are required to have policies related to the access of patient charts. Perioperative personnel must follow these policies to ensure patient privacy and the security of electronic records.
(ORNAC, 2021 – 3.10)
Making Changes to Documentation
Although most charting is performed using computer systems in the perioperative environment, there is documentation that remains paper-based, such as count sheets. Perioperative nurses must follow the health care organization’s specific policy for correcting paper and computer entries. This could include:
- Drawing a single line through an incorrect entry.
- Dating and timing the change.
- Initial correction.
- Entering the correct information.
(ORNAC, 2021 – 3.10)