Movement in the Operating Room
Movement around the sterile field should be limited:
- Scrubbed personnel should remain close to the sterile field.
- When moving around other scrubbed personnel, they must pass back-to-back or face-to-face.
- Non-scrubbed personnel must always face the sterile field to observe and ensure they have not caused contamination.
- Non-scrubbed personnel must remain at least one foot away from all sterile tables/items.
- Non-scrubbed personnel must not walk between two sterile fields.
All members of the surgical team are responsible for adhering to and ensuring sterile technique.

Monitoring the Sterile Field during Surgical Delay
The sterile field should be set up as close to the start of surgery as possible. Occasionally a delay will occur after the sterile field has been set up. In these instances, the OR team must have a member monitor the sterile field to ensure it has not become contaminated.
The sterile field should never be left unattended as contamination could occur from:
- Other personnel
- Airborne contaminants
- Liquids
- Insects
(King & Spry, 2019; ORNAC, 2021).
The sterile field can be covered if there is an identified risk of contamination such as:
- An extended delay was not anticipated.
- Moments of increased activity in the OR such as transferring a patient or bringing equipment into and out of the OR, or a code blue situation when additional personnel are present.
- Any time when the heating, ventilation, or air conditioner system (HVAC) is disrupted. That may cause accumulated dust or debris to be circulated when the system starts up again.
- If the sight of instrumentation is disturbing to the patient or family member present for induction.
The perioperative nurse must properly uncover a sterile field by reaching a cuffed portion of the drape and bringing it downward to prevent any area that had hung below the table from being dragged across the surface.
(ORNAC, 2021 – 2.17)
🧩 Practice Activity: What to do if Contamination Occurs
Use the previous and next buttons to navigate through questions. Select “Check” when you feel confident in your answer. When you have completed all the questions, select the “Finish” button.
(ORNAC, 2021 – 2.1).
📽️ AORN CINE-MED VIDEO
Navigate to the AORN Cine-Med website and make sure that you are logged in before clicking on the link below.
- Watch the AORN Cine-Med Video on: Sterile Technique: An Introduction
- Download the Study Guide included to follow along.
- (Thread to follow in Cine-Med – Aseptic Practices Sterile Technique: An Introduction)
- Runtime – 26 minutes
Hand Washing Scrub and Solution
Hand hygiene refers to the practices implemented by personnel to decontaminate hands using soap and water or an alcohol-based waterless solution.
Surgical Hand Asepsis is the term used when someone prepares to ‘scrub in’ and will be donning sterile gloves and a surgical gown. Surgical hand asepsis cannot make skin sterile, but it is used to reduce the risk of SSI (Surgical Site Infection) for the patient by removing and suppressing the growth of microorganisms on the skin.
Before beginning surgical hand asepsis, scrub personnel must:
- Ensure proper fit of mask and eye protection prior to beginning scrub or rub.
- Ensure all jewelry has been removed from hands and wrists.
- Ensure the skin is free from open lesions and breaks in skin integrity, as these can be a potential source of infection for both the patient and scrubbed personnel.
(King & Spry, 2019; ORNAC, 2021 – 2.12).
Explore the scrub sink environment by selecting the arrows and click/drag to move front view.
Surgical Hand Scrub
Surgical hand scrubs are the more traditional method of performing hand asepsis using an antiseptic agent and water. Key ORNAC Standards include:
- Nail cleaners should be used to clean under fingernails for the first scrub of the day. (ORNAC Standard 2.12.6)
- Water scrub – Hands should be held above the elbows and away from surgical attire. The direction of the scrubbing procedure is from fingers to elbows without returning to the cleaned hands. (ORNAC Standard 2.12.8)
- Water scrub – Either a prescribed TIME or number of STROKES must be used with friction. (ORNAC Standard 2.12.9)
- Water scrub – Hands and arms shall be dried with a sterile towel prior to gowning. (ORNAC Standard 2.12.10)
(King & Spry, 2019; ORNAC, 2021).
🧩 Practice Activity: Basic Steps of Surgical Hand Scrub
Click and drag the image blocks into the correct order. Select “Check” when you feel confident in your answer. When you have completed all the questions, select the “Finish” button.
(King & Spry, 2019; ORNAC, 2021 – 2.12).
Drying
After performing surgical hand asepsis using the water-based scrub method, personnel enter the OR room using their back to open the door and maintaining arms bent at elbows in front of the body.
The circulator can open the gown pack on a flat surface to create a sterile surface. This should be separate from the surgical back table to prevent contamination of the sterile setup.
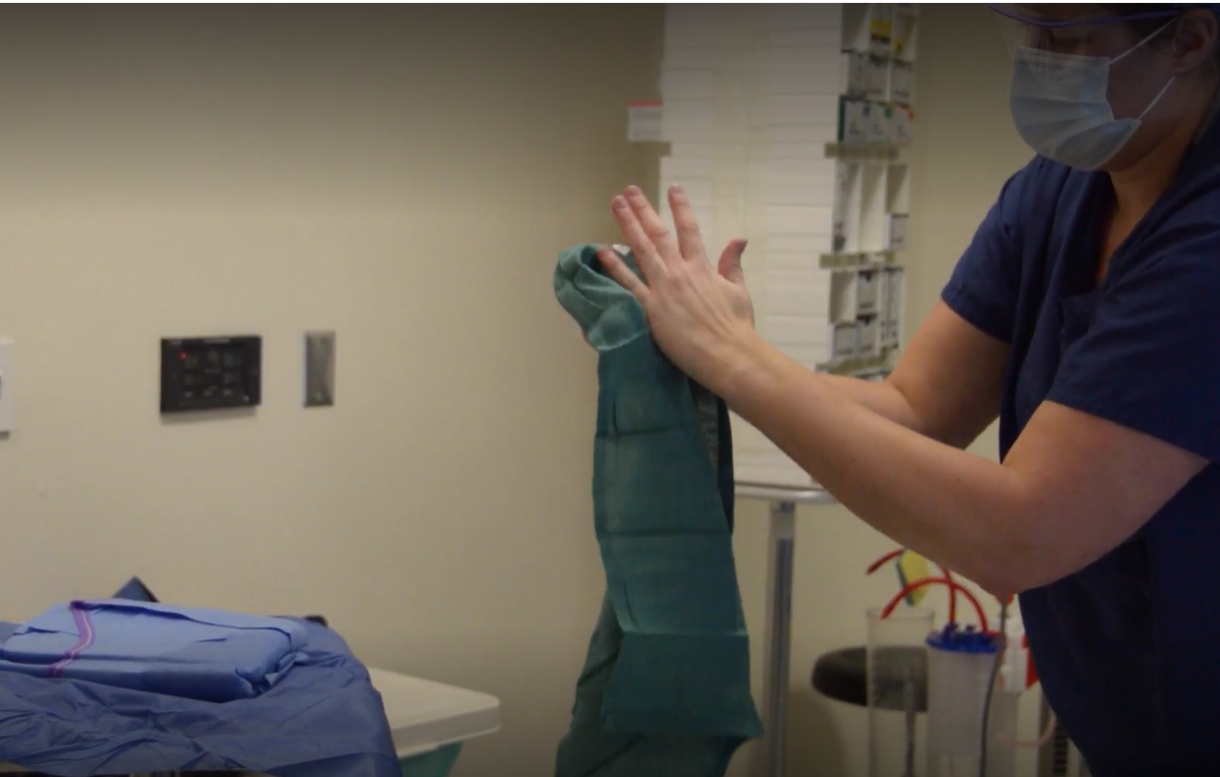
- A paper or cloth towel is included with the surgical gown pack.
- Scrubbed personnel reach over the open gown pack and grasp a corner of the towel, lifting it straight up and away from the sterile field so as not to drip water and contaminate the gown.
- The scrubbed person steps back from the gown pack and leans slightly forward at the waist keeping arms bent at the elbows.
- Allowing the towel to unfold, the scrubbed person can visually divide the towel in half (one half for each arm).
- Using the hand holding the towel, the scrubbed person uses the top half of the towel to blot the opposite arm dry.
- This process moves from the cleanest area (hands) to the dirtiest (elbows) beginning with the fingers, then the palm, and finally the forearm. It is important to move in one direction and not cover an area more than once.
- Once the arm is dry, the process is repeated for the other arm, using the clean half of the towel.
- Once completed, the towel can be discarded while maintaining arms above waist height.

Alcohol-Based Hand Rub
Surgical hand rubs are easy to use and fast-acting. Follow the manufacturer’s guidelines for use. Usually, hand washing with soap and water, as well as cleaning under nails with nail cleaner, are required before applying rub for the first scrub of the day, or if hands are visibly soiled.
KEY ORNAC Standards for applying alcohol-based rub include:
Waterless scrub – Allow agent to completely dry according to the manufacturer’s directions before donning the sterile gown and gloves (ORNAC Standard 2.12.11)
(King & Spry, 2019; ORNAC, 2021 – 2.12).
🧠 Graded Activity
In Blackboard, complete the Graded Activity: Handwashing.
Considerations when Donning a Sterile Gown
Sterile gowns and gloves are used to create a barrier which prevents microorganisms from the scrubbed personnel from entering the surgical site. Gowns and gloves also act as a barrier to protect scrubbed personnel from contact with a patient’s bodily fluids.
Surgical gowns can be made of cloth and reusable, or disposable. They can be rated to withstand varying degrees of stress/exposure. Appropriate gowns are determined based on the surgical procedure and exposure to fluids. They must be combustion resistant and provide an adequate barrier from microorganisms.
Key Features of Surgical Gowns:
- They must provide a good fit for the scrubbed personnel, allowing them to move easily.
- They should provide reinforcement from the waist up and over the forearm sleeve area.
- All sleeves should include a tight-fitting cuff that helps to stop them from moving up or down.
- They must be secured at the back.
- Wraparound gowns are recommended to help provide additional coverage of the scrubbed person’s back.
- Gowning should always take place away from the back table on a separate sterile surface to prevent contamination.
- Gowns are packaged in a way that the scrubbed personnel can pick them up without touching the outside aspects to maintain sterility.
(King & Spry, 2019; ORNAC, 2021 – 2.13).

Methods of Donning Sterile Gloves


Considerations when Donning Sterile Gloves
Due to increased latex sensitivity for both patients and perioperative personnel, many institutions have moved away from using latex gloves.
When selecting the appropriate gloves, it is important to consider the following:
- The length of the surgery.
- The type of procedure being performed.
- The need to wear double gloves.
- Will the gloves be exposed to stress, such as with reamers and drills?
- Will there be any chemical or medication exposures during the procedure?
- Are there any latex or other sensitivities for the patient or perioperative personnel?
- The preference of the perioperative personnel.
(King & Spry, 2019; ORNAC, 2021 – 2.14).
🧩 Practice Activity: Steps for Gowning and Closed Gloving
Read the description of each image by clicking the ellipsis (…) Click and drag the image blocks into the correct order. Select “Check” when you feel confident in your answer. When you have completed all the questions, select the “Finish” button.
Use the scrollbar to reveal the image sequence.
Once the gloves are in place, the scrubbed person can detach the cardboard tab on the front of the disposable gown or untie the straps on a reusable gown and wrap the strap in the paper glove wrapper. They then pass the carboard tab to the circulator (or the strap wrapped with the glove wrapper). They then slowly turn so the gown wraps around the back of the scrubbed person. Once turned around, the scrubbed person pulls on the strap to detach the cardboard and leaves it with the circulator. The scrubbed person can then secure the side strap in place.
(King & Spry, 2019; ORNAC, 2021 – 2.13; 2.14).
Steps for Assisted Gloving
Step 1: The scrubbed person who is already gowned and gloved, removes one glove from the package (general rule is to always start with the right).
Step 2: They place fingers from both hands beneath the everted cuff and keep thumbs turned outward.
Step 3: The scrubbed person then presents the open end of the glove toward the person being gloved. This is done by stretching the cuff outward using the cuff to protect their hands, while the other person slides their hand into the glove in a downward direction.
Step 4: This method can also be used when a scrubbed team member’s glove is contaminated.
- In this case, the circulator dons nonsterile gloves and pinches the centre of the contaminated glove, pulling it off in a downward direction away from the scrubbed person.
- The scrubbed person may not pull their hand back inside the cuff of the gown as a cuff is not considered sterile.
- They then follow the steps for assisted gloving to don a new pair of sterile gloves.
(King & Spry, 2019; ORNAC, 2021 – 2.13; 2.14; 2.15).
When Should Sterile Gloves be Changed?
Sterile surgical gloves should be changed:
- After contact with a patient.
- Whenever a defect, a hole or tear is noted.
- Anytime suspected contamination has occurred.
- If a glove is punctured by a needle, suture, or any other sharp item.
- Immediately after using methyl methacrylate which is commonly used in bone cement.
- Before handling an implant.
- If an unintentional electric shock occurs from the electrocautery device.
- If gloves begin to swell or become loose.
- According to any protocol or policy at the institution. Many institutions have enacted clean closure protocols which require gloves to be changed after working in a contaminated area such as in bowel anastomosis.
(ORNAC, 2021 – 2.15).
Sterile Areas of Scrubbed Personnel
When someone has scrubbed and donned a sterile gown and gloves, it does not mean that they are now sterile from head to toe. In fact, there are specific areas of a scrubbed person’s body that are considered sterile based on their ability to maintain and monitor for contamination.
✔️
Sterile
- Front of gown chest to the level of the sterile field. This is different for people of different heights.
- Scrub personnel should avoid changing the level of the sterile field when standing on a footstool or sitting. The only time that a scrub person should be seated is if the entire procedure takes place seated.
- Sleeves – two inches above the elbow to the cuff down to the sterile gloves, not including the cuff of the gown.
- Gloves are considered sterile. Sterile gloves must extend past the sterile gown cuff to cover it.
❌
Not Sterile
- The gown cuff is not considered sterile and must be covered by sterile gloves.
- The neckline, shoulders, axillary area, and back are not considered sterile. A wraparound gown can be considered sterile when being put on; however, because the scrub personnel cannot observe and protect it from contamination, it does not maintain sterility.
- Quick quiz. Which images demonstrate proper sterile technique?
(King & Spry, 2019; ORNAC, 2021 – 2.13).
🧩 Practice Activity: Scrubbed Personnel
Use the previous and next buttons to navigate through questions. Select “Check” when you feel confident in your answer. When you have completed all the questions, select the “Finish” button.
Removing Sterile Gown and Gloves
- When removing cloth gowns, the circulator should untie the straps behind the scrubbed person. The scrubbed person can untie the side strap.
- The scrubbed person should then turn the outer side of the soiled gown away from themselves and roll the gown down their arms.
- The scrubbed person pulls the gown over their hands and places it in the linen hamper if cloth, or the garbage, if disposable.
- To remove gloves without contaminating themselves, the scrubbed person slides the gloved fingertips along the palm of the opposite hand until the fingers reach the cuff. They pinch this cuff and pull the glove off the hand (glove-to-glove).
- For the second hand, they slide the unloved hand underneath the remaining glove and slide it off (skin-to-skin).
(King & Spry, 2019; ORNAC, 2021 – 2.15).
📽️ AORN CINE-MED VIDEO
Navigate to the AORN Cine-Med website and make sure that you are logged in before clicking on the link below.
- Watch the AORN Cine-Med Video on: Hand Hygiene, Scrubbing, Gowning and Gloving
- Download the Study Guide included to follow along.
- (Thread to follow in Cine-Med – Aseptic Practices Hand Hygiene, Scrubbing, Gowning and Gloving)
- Runtime – 31 minutes