Prevention of Surgical Site Infections
Surgical site infections (SSIs) are one of the most common complications in surgical care. SSIs can increase patient morbidity and cost hospital organizations valuable resources to treat an infection that could have been prevented. SSIs can occur at the skin/surgical incision level or originate deep in incisions, cavities, or organs. SSIs have many different causes which can be divided into patient-related or extrinsic factors.
Infections are classified as SSIs if they occur at the surgical incision site. They can develop within 30 days of a surgical procedure or even up to a year if there was an implant, such as a knee or hip joint implant.
(King & Spry, 2019)
Microorganisms in the OR
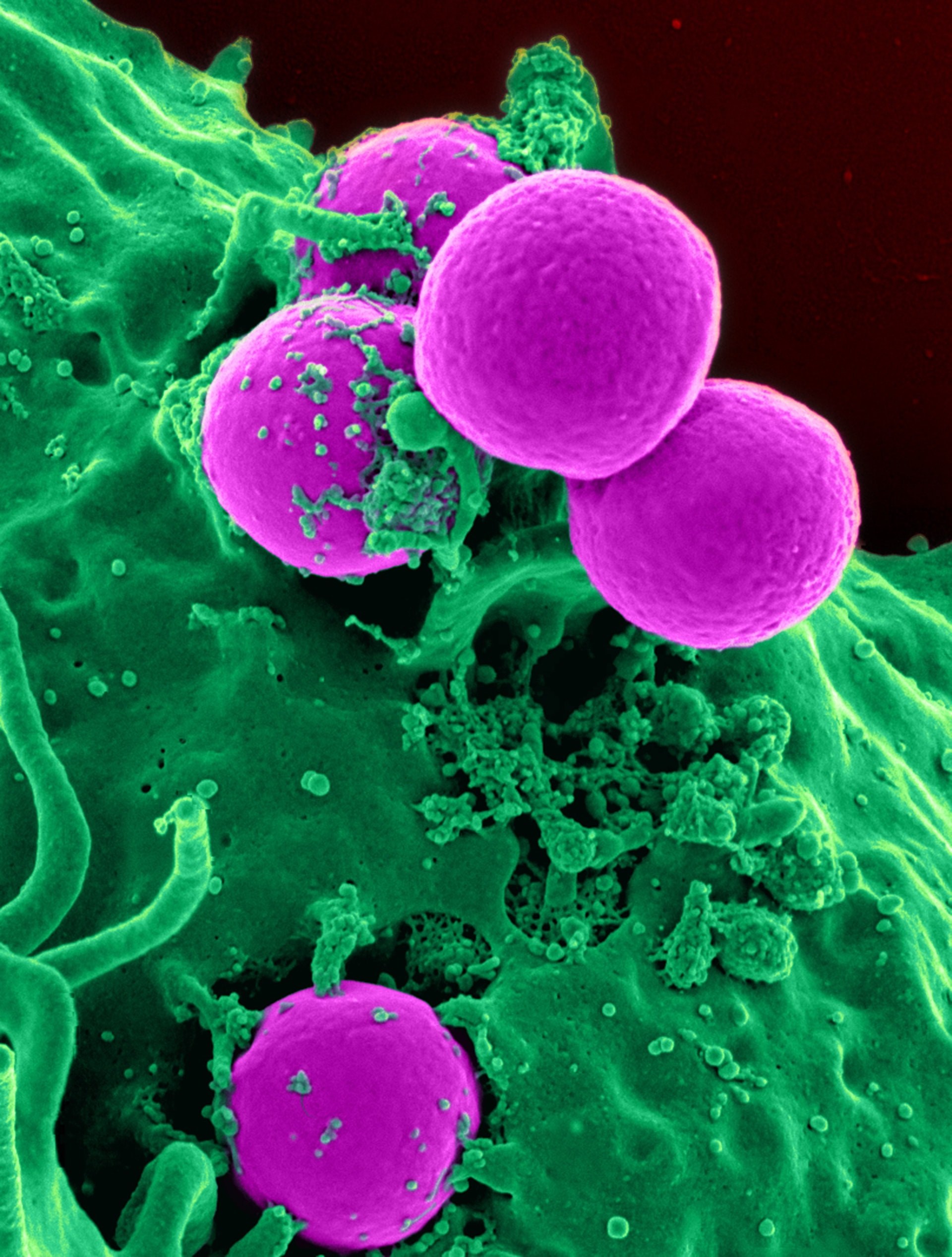
Any organism that can cause infection can cause an SSI (Surgical Site Infection); however, most SSIs can be traced back to organisms that are normal flora on a patient’s skin. Modern methods of disinfection can reduce but not eliminate endogenous organisms on a patient’s skin. Because some organisms reside in the hair follicles and sebaceous glands which cannot be reached with topical surgical prep, some of these structures are transected bringing these organisms into the surgical wound when an incision is made. Not all SSIs are caused by a patient’s normal flora. Microorganisms can enter a surgical site through contaminated instruments, shedding from the skin, mucous membranes, or clothing of perioperative personnel.
Microorganisms that Cause Infection:
(King & Spry, 2019)
Infections
Infection – An infection occurs whenever non-resident florae or microorganisms invade a susceptible area of the body. There is a reaction of the tissues to the microorganism’s presence and toxins are generated by the organism.
Superinfections – These occur after a patient has been treated with antibiotics and a secondary subsequent infection develops, caused by a different microorganism.
(Phillips, 2020)
Bioburden and Biofilm
Because it is not possible to sterilize a patient’s skin when using skin prep, there is always a chance that some microorganisms could be present near or at the surgical site.
Bioburden is the amount of microbial load or organic debris that can be found on something. This could include a host, such as a patient’s skin, or an inanimate object, such as a surgical instrument before it is sterilized.
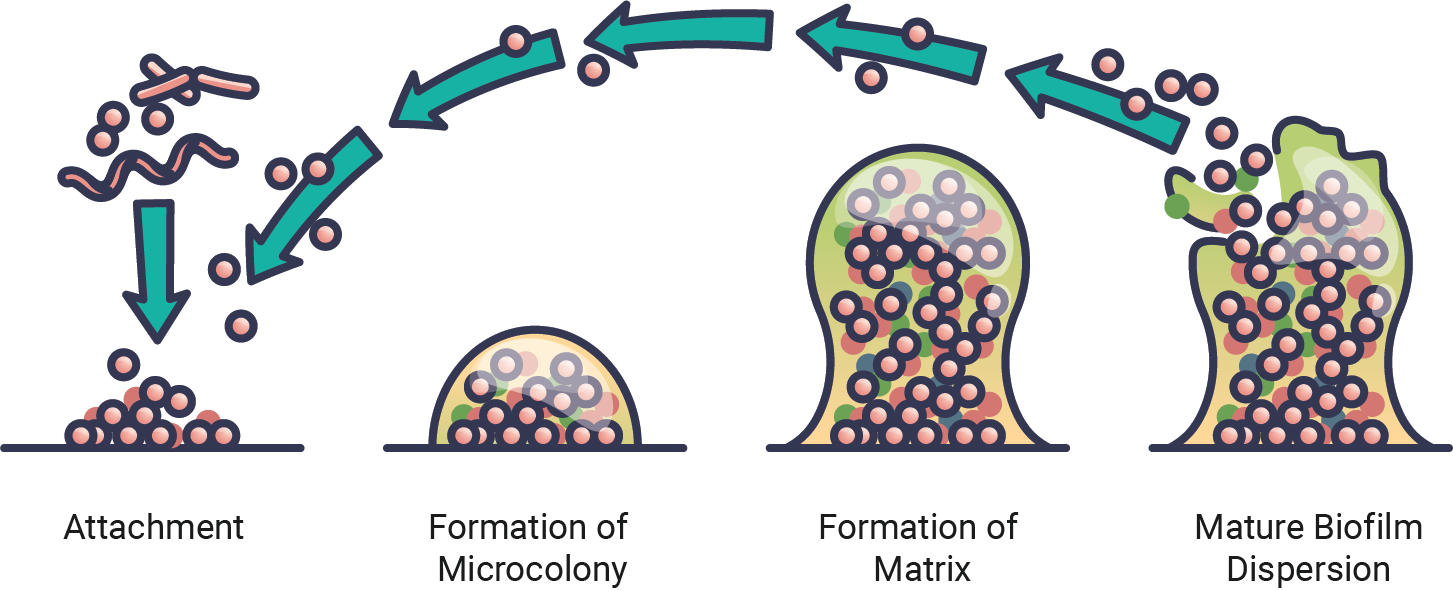
Biofilm is the thin coating on an item or host that contains biologically active organisms that can grow in water, solutions, or in vivo. These organisms can coat the surface or structure of devices and can be trapped within organic matter.
Consider how organisms on surgical instruments may allow for biofilm build-up during a case. These organisms may then be detached and dispersed into the surgical site.
(Phillips, 2020)
Chain of Infection
Follow the chain of infection to understand how infectious agents gain access to a susceptible host:
Breaking the Chain of Infection
Because a surgical site provides an easy portal of entry for an infectious agent, antimicrobial agents are used in the perioperative environment to help break the chain of infection and prevent or reduce the risk of surgical site infections (SSIs).
Routes for Administration of Antimicrobial AgentsPO (oral) administration preoperatively or postoperatively can be given therapeutically or prophylactically:
- Therapeutically – to eliminate organisms during an infection
- Prophylactically – to prevent the development of an infection
(Phillips, 2020)

🧩 Practice Activity: Prophylactic Antibiotic Use in the Operating Room
Complete the activity by dragging the text block into a drop zone. Select “Check” when you feel confident in your answer(s).
Common Organisms which can cause SSIs
Review the common microorganisms found in the OR.
Based on the chart you just reviewed, you can see that various surgical procedures place patients at higher risk for an SSI from a specific bacteria or microorganism. For this reason, if preoperative antibiotics are recommended, the surgical team will choose antibiotics as a prophylaxis to specifically target the causes of infection.
Preventing SSIs… Antibiotic Stewardship
Antibiotic resistance is a growing worldwide problem and is one of the biggest threats to global health. Perioperative team members have a role to play in ensuring that antibiotics are only dispensed and given when required. Perioperative team members must also ensure they prevent infections by adhering to strict hand hygiene and cleaning/ sterilizing perioperative instrumentation and environments.
Patients who are undergoing surgery where antibiotic prophylaxis is recommended, need to receive the following:
- The right type of antibiotic is based on the surgery being performed and patient characteristics such as allergies.
- The right dose is based on the patient’s weight.
- The right time. The initial dose is usually administered within one hour of the first incision. Additional intraoperative doses may be required based on the length of surgery and estimated blood loss.
- The right length of treatment. Prophylactic post-op antibiotics should not be given for longer than 24 hours. Limiting the duration of postoperative prophylactic antibiotic therapy may lead to reductions in antibiotic use and in Clostridium Difficile infection.
(Public Health Ontario, 2019; WHO, 2020)
Surgical Antibiotic Prophylaxis Optimization
An audit of quality indicators for surgical antibiotic prophylaxis to identify areas that need improvement.
Read Article
Resistance to Antibiotic Therapy
Managing new and emerging microorganisms significant in the perioperative environment
📽️ AORN CINE-MED VIDEO
Navigate to the AORN Cine-Med website and make sure that you are logged in before clicking on the link below.
- Watch the AORN Cine-Med Video on Environmental Cleaning and Autologous Tissue Management
- Download the included Study Guide to follow along.
- (Thread to follow in Cine-Med – Patient and worker safety Environmental Sanitation, Terminal Cleaning, and Disinfection)
- Runtime – 36minutes