Environmental Cleaning
A clean, safe environment is vital to providing excellent perioperative patient care. There are different practices have been implemented to prevent the transmission of microorganisms in the perioperative environment. These include:
- Wearing proper surgical attire.
- Establishing and following controlled traffic patterns in the perioperative environment. This includes limiting traffic inside an OR and limiting the use of the operating room doors. These measures help perioperative team members to decrease air turbulence and reduce human shedding.
- Limiting the OR equipment to only that which is essential.
- Keeping operating room doors closed except to pass equipment through. This helps to maintain the positive pressure environment required in the operating room.
- Having HEPA filters to clean the air entering the operating room space can screen out any particles that are larger than 0.3 µm.
- Having designated cleaning practices. policies and procedures in place to identify exactly: what needs to be cleaned; how it should be cleaned; when it needs to be cleaned; and who needs to clean it.
(King & Spry, 2019; ORNAC, 2021)

Specifics of the OR Environment
The OR environment must be designed with infection prevention in mind. Click on the OR areas to learn more about the design features in preventing the spread of infection and find the following:
- Central Core
- Floors
- Walls
- Doors
- Cabinets
- Scrub Sinks
- Soiled Workspace
(King & Spry, 2019)
Temperature and Humidity in the OR Environment
Temperature and humidity levels are important in the OR environment.
Temperature
- ORNAC standards recommend that the OR should be maintained between 20-23°C.
- Exceptions include pediatric patients, burn patients, geriatric patients, and patients experiencing hypothermia.
Humidity
- The operating room humidity should be between 30-60%. This helps to reduce static electricity which can be present when humidity is low. It also helps to reduce dust accumulation which can increase when humidity is low.
- There is a potential for bacterial growth which can occur when humidity is high.
- There is also a potential for condensation and moisture buildup on supplies which can occur when humidity is high.
(King & Spry, 2019, ORNAC, 2021)

Air Pressures in the Operating Room
Airflow and pressures in the operating room are important aspects of infection prevention.
Air pressures in the OR must be greater than pressures outside. This creates a ‘positive pressure’ environment which helps to maintain a unidirectional airflow. This prevents air in the corridors from entering the OR. The outside air may contain microorganisms.
There is one exception when surgical procedures are performed on a patient with an airborne infection such as TB or measles. In that case, the OR can switch to negative pressure for infection prevention measures.
The direction of airflow in the OR is also important in preventing infections. All airflow should enter the OR at the ceiling level (see rectangle vents in the top right image) and follow a downward flow to be exhausted at the floor level (see corner exhaust in the bottom right image).
ORNAC standard 4.4 requires that each OR have a minimum of 20 air exchanges each hour, with at least six clean air exchanges with air drawn from outside.
(King & Spry, 2019, ORNAC, 2021)


General Practices
Cleaning practices can be broken down into:
- Routine
- Enhanced
- Terminal
(King & Spry, 2019, ORNAC, 2021)
Routine Cleaning Before, During and After Each Surgical Case

Additional Cleaning Measures
Additional cleaning takes place routinely on a weekly and monthly schedule to ensure the operating room environment remains clean. Project cleaning is another term used when special cleaning practices occur. Institutions should develop and post the cleaning schedules clearly, noting their frequency and timing so that areas are not missed.
Items to be cleaned can include:
- Ceilings and walls, including recessed ceiling tracks
- Floors which should be power scrubbed at regular intervals according to the health care organization’s policy/procedures
- Air conditioning and ventilation grills
- Light fixtures
- Sprinkler heads and other fixtures
- Ducts and filters
- Cabinets, closets, shelves, and warming cupboards
- Storerooms
(ORNAC, 2021)
Terminal Cleaning: End of the Day Cleaning
At the end of the surgical list, a terminal clean is conducted. This includes all cleaning aspects conducted between cases/turnover, as well as giving specific attention to:
- Surgical lights and external ceiling mount tracks
- Air ducts and intake grills
- Door handles, cabinets, and push plates
- Light switches and controls
- Telephones, as well as computer keyboards and screens
- Walls – by spot-checking for cleanliness
- Exterior surfaces of all machines and equipment, allowing adequate drying time, as per manufacturer’s IFU (Instructions for Use), before storage
- Furniture, including wheels/casters
- Horizontal surfaces
- Scrub sinks, faucets, and surrounding walls
- Kick buckets, garbage, recycling, laundry receptacles, and frames
- Floors must be cleaned thoroughly
(ORNAC, 2021)
Enhanced cleaning – Practices for additional precautions
When a patient is suspected of having an infectious illness, enhanced precautions are put in place. These provide additional safety for healthcare providers and prevent the spread of the illness. Enhanced cleaning measures will also take place when the patient leaves the operating room.
- Specific cleaning practices are noted under the enhanced precaution measures.
- Depending on the infectious illness, different cleaning solutions may be required, Examples are AROs including MRSA, VRE, carbapenems-producing Enterobacteriaceae (CPE), c-diff, TB, and prion disease (e.g., CJD).
In these cases, a terminal clean will be performed which integrates special disinfectants which target specific microbes.
(ORNAC, 2021)
Workplace Hazardous Materials Information System (WHIMIS)
The perioperative environment utilizes many different chemicals and cleaning solutions to ensure a safe patient environment. Because of this, all perioperative personnel must be trained in and understand the safety measures when working with hazardous materials.
Institutions are required to follow and comply with Workplace Hazardous Materials Information System (WHMIS) regulations and follow safety policies and procedures. All personnel must receive regular training in WHMIS regulations and follow the protocols to ensure a safe environment of care.
For more information check out https://whmis.org/
(ORNAC, 2021)

Environmental Responsibility in the OR
Perioperative personnel have a responsibility to look for ways to prevent waste. Following the 4Rs – Reduce, Reuse, Recycle and Recover – perioperative personnel can do their part to decrease the OR’s impact on the environment.
- Reduce: Reduce waste by not opening ‘as needed /PRN’ supplies until they are required. This cuts down on waste and saves healthcare dollars.
- Reuse: As much as use reusable items instead of sole use disposable equipment.
- Recycle: Use any clean paper or plastic materials that are recyclable, if they are not contaminated by any biohazardous materials.
- Recover: Transform waste into resources. This can be demonstrated in the OR breakroom by composting.
Routine Practices
The purpose of routine practices, also known as standard precautions, is to reduce the transmission of microorganisms from sources of infection, which can be known or unknown.
Health Care providers MUST consider that any patient could be infectious, even if they are not symptomatic. For this reason, it is important to assess the risk of exposure to bodily fluids including blood, secretions or excretions, mucous membranes, and non-intact skin.
🧩 Practice Activity: Quick Quiz
Choose one or multiple responses to answer the question. Select “Check” when you feel confident in your answer.
Hand Hygiene
This is the number one method of preventing the spread of infection:
- Proper hand hygiene is the responsibility of ALL health care providers.
- It is preferable to clean hands using an alcohol-based hand rub if hands are not visibly soiled. If visibly soiled, hands must be washed with soap and water.
- Healthcare team members must follow the 4 moments of Hand Hygiene. Review the image to reinforce these 4 moments.
(King & Spry, 2019, ORNAC, 2021)
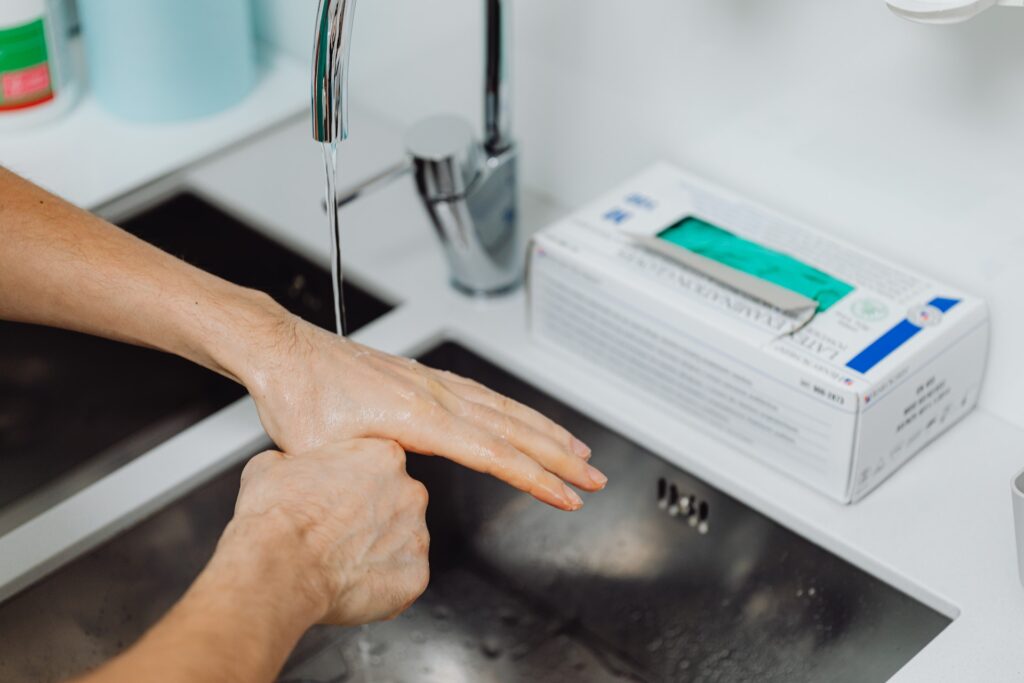
Your 4 Moments for Hand Hygiene
The steps for hand hygiene throughout the surgical environments (select the + hotspots in the image to reveal information):
Source: Public Health Ontario